Again, I am lucky. Another day no side effects. I am truly pleased that I am keeping this diary so that you can see how I have coped. As I have already said, Pre-2017, PEP medication side effects sounded brutal! Almost guaranteed diarrhea, nausea, and headaches on most days over the course of the 30 days you need to take the meds. In 2017, the two pill a day cocktail you now have to take, reportedly, has the same symptoms, but to a far lesser extent. I say reportedly because I write this now on day 13 of the medication. This blog constitutes my daily diary as I go through the 30 days of PEP treatment. I expect different people will have different reactions/ experience different side effects, so, to help you gauge how similar yours might be to mine, I will tell you about me. I’m 182cm tall, and white European (52% English, 46% Spanish, 2% Sicilian) according to recent DNA test results. I have no allergies, never had any STI/ STDs before, I’m fit and healthy, 29 years old, weigh 79kg, and am uncircumcised. Apparently having that bit of extra fleshy penis protection still attached equates to having a large mucosal surface membrane through which the HIV transfer could occur.
What is PEP?
PEP, or post-exposure prophylaxis is a 4-week course of anti-HIV drugs that are taken shortly after possible exposure to HIV infection. Taking the drugs may help reduce the risk of acquiring HIV if you have an exposure to the virus.
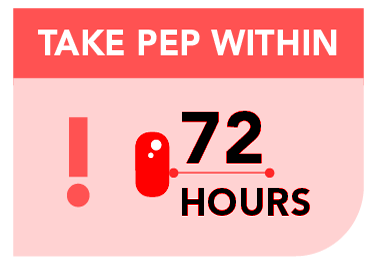
When should I take PEP?
It is recommended that PEP be started as soon as possible after the exposure to HIV – preferably within a few hours. This gives the drugs the best chance to work against HIV before it becomes established in the immune system. PEP should be started as soon as possible but may be taken up to 72 hours after the exposure.
Who should take PEP?
Anyone who has had risky contact with a person who has HIV, or who may have HIV, should consider taking PEP. This risky contact may include unsafe sex, sharing injecting equipment, needlestick injury or other blood exposure. It is important to discuss the need for PEP with a health care provider trained in using anti-HIV drugs, or with clinical staff at a hospital Emergency Department. Together, you can determine your risk of acquiring HIV and decide whether you should take PEP. If you are pregnant, think you might be pregnant, or are breastfeeding, discuss this with your health care provider before starting PEP.
What is involved in taking PEP?
PEP involves taking a 2 or 3 drug combination once or twice daily for four weeks. The drugs need to be taken at certain times of the day and may need to be taken with food. It is very important not to miss any doses of PEP to give it the best chance of working. If seen at an Emergency Department or Canberra Afterhours Locum Medical Service (CALMS), you will be given a starter pack so you can commence PEP immediately. This pack only has enough pills for a few days. To continue PEP, you will be referred to a doctor or sexual health centre for a script for ongoing supply.
Does PEP have side effects?
Yes. Taking drugs used in PEP can cause side effects such as nausea, diarrhoea, headaches, tiredness and a rash. Rarely, more serious side effects have been reported. You should discuss the possible side effects and how to manage them with your health care provider.
Will I need blood tests?
If you decide to take PEP, “baseline” blood tests will be done to check your current status for HIV, hepatitis B and C. Tests for other sexually transmitted infections (STIs) may also be recommended, either when you are prescribed PEP, or at your follow up visits.
Does PEP work?
Studies done with health care workers show that their risk of becoming HIV positive after a needlestick injury is significantly reduced by using PEP. These studies suggest that it is also possible to reduce the risk of getting HIV by prompt use of PEP after possible sexual or injecting exposure. PEP will NOT COMPLETELY ELIMINATE this risk.
Do I still need follow up after completing PEP?
Yes, follow-up is very important. If you take PEP, blood tests for HIV are repeated at these times after the exposure: at 6 weeks and again at 3 months
What else do I need to know while taking PEP?
- PEP is not guaranteed to stop you from being infected with HIV and it is not a replacement for safe sex and safe injecting practices
- Taking PEP will not make you immune to HIV
- Women should use effective birth control to avoid pregnancy whilst on PEP
- HIV testing will need to be repeated at 3 months after you commence PEP. This is called the window period (the time it can take for HIV to show up in tests). You need to protect others during the 3 month window period by using condoms, and not sharing injecting equipment
- Do not donate blood, sperm, organs or tissue while on PEP and within the 3 month window period
- If you miss a tablet, take the dose as soon as you remember and seek advice by calling your GP, sexual health service or the PEP Hotline as to how you should continue to take the drugs